Contact tracing, as implemented by the Centers for Disease Control and Prevention (CDC), is a public health strategy aimed at controlling the spread of infectious diseases systematically. This process involves several steps like identifying confirmed or suspected cases, interviewing these individuals to ascertain their recent contacts, notifying those contacts of their potential exposure, and advising them on appropriate measures such as testing, symptom monitoring, and quarantine or isolation to prevent further transmission.
Traditional methods of contact tracing involve collecting minimal personal information, such as names, contact details, and health status, while avoiding unnecessary disclosure of the infected individual’s identity to their contacts. For example, in manual contact tracing, public health workers separate case investigation from contact notification to prevent inadvertent exposure of the index case’s identity.
According to a study on the future of the practice ‘Digitalization of contact tracing: balancing data privacy with public health benefit’ published in the Ethics of Information Technology, “Effective use of digital case management for contact tracing requires revisiting the existing legal frameworks, privacy protections, and security practices for management of sensitive health data.”
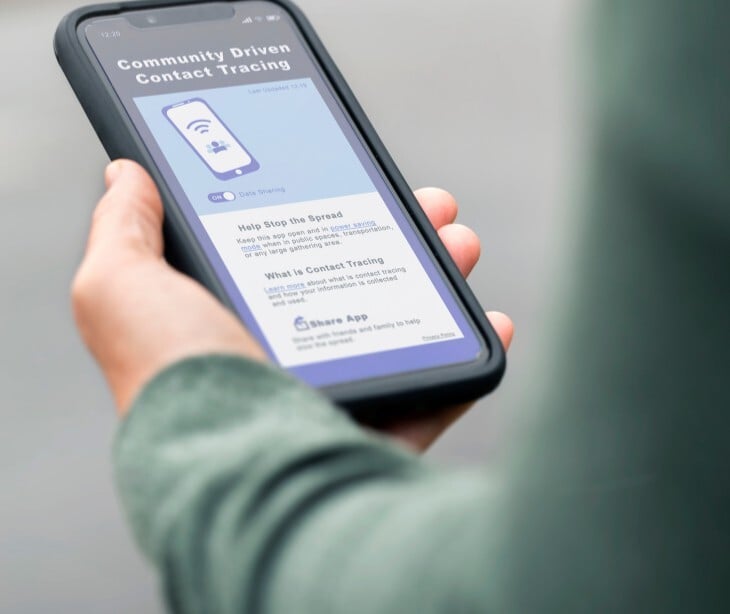
Digital case management systems further complicate privacy concerns, as scaling operations requires data security practices to prevent breaches. The study also provides, “Contact tracing during the pandemic has gained particular attention for the new use of digital technologies—both on the consumer side in the form of Exposure Notification applications, and for public health agencies as digital case management software systems enable massive scaling of operations.”
While HIPAA governs protected health information (PHI) in clinical settings, its applicability to contact tracing is limited. PHI collected during contact tracing often falls under public health exemptions in HIPAA, allowing agencies to use data for disease control without individual consent.
The CDC’s methodologies and protocols for contact tracing
The CDC’s contact tracing methodologies emphasize timeliness, accuracy, and integration with broader public health strategies. During the Ebola outbreak, protocols focused on identifying all contacts of confirmed cases, monitoring them for 21 days, and isolating symptomatic individuals promptly.
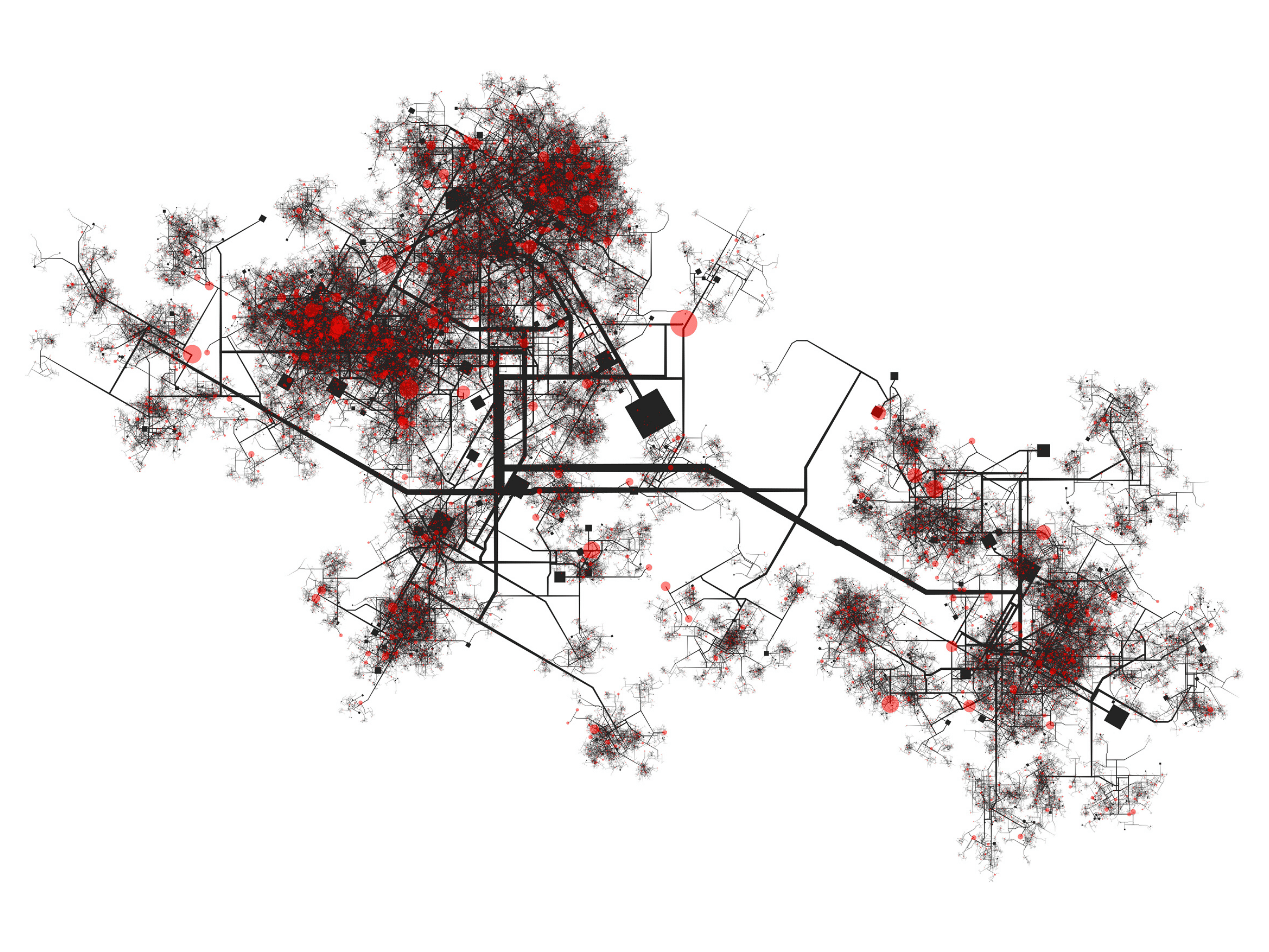
A JMIR Public Health and Surveillance study ‘Effectiveness of Contact Tracing for Viral Disease Mitigation and Suppression: Evidence-Based Review’ on contact tracing in viral disease mitigation notes, “Approaches to contact tracing have traditionally used telephone and in-person communication; however, newer approaches examine the use of mobile apps and leveraging data to track and trace social connections and potential exposures.” For COVID-19, the CDC adapted these principles to address higher transmission rates, advocating for a combination of case interviews, digital tools, and collaboration with local health departments.
Steps include:
- Case investigation: Interviewing infected individuals to identify contacts and exposure settings.
- Contact notification: Informing contacts of potential exposure while maintaining confidentiality.
- Quarantine and monitoring: Recommending isolation for exposed individuals and daily symptom checks.
The CDC also promotes combination interventions, where contact tracing is paired with masking, testing, and vaccination to reduce transmission. In healthcare settings, protocols involve centralized teams using EHRs and human resource data to trace exposures among staff and patients, often requiring rapid risk assessments and workflow adjustments. Challenges include scalability during surges and ensuring compliance, particularly in communities with mistrust of public health authorities.
The value of contact tracing through the lens of past health crises
A journal article from the American Public Health Association on the history of contact tracing and potential direction of public health states, “A recent review by El-Sadr et al.1 traces the use of contact tracing for syphilis and gonorrhea, tuberculosis, HIV, Ebola, and, most recently, COVID-19. A wide range of approaches, however, fall within the general rubric of contact tracing. These strategies have been based on the authority of the state to surveil and track epidemics; require physicians and public health agencies to report certain diseases; and identify individuals for surveillance, investigation, and contact by public health authorities.”
During the 2014 Ebola epidemic, rigorous contact tracing in West Africa helped isolate cases and reduce transmission chains, demonstrating its effectiveness in low-resource settings. For HIV, contact tracing evolved into partner notification services, balancing privacy concerns with the need to interrupt transmission.
The COVID-19 pandemic revealed its adaptability, digital tools enabled mass scaling, while traditional methods remained necessary in underserved areas with limited technology access. Historically, contact tracing has also driven shifts in public health philosophy. Early efforts, such as syphilis control in the 1930s, relied on coercive state authority, whereas modern approaches emphasize community engagement and support (e.g., providing isolation resources).
Is the contact tracing data considered PHI
Contact tracing data qualifies as PHI when it is linked to identifiable individuals and held by HIPAA-covered entities (e.g., healthcare providers). For example, EHR entries documenting a patient’s exposure history are PHI. However, public health agencies are exempt from HIPAA’s restrictions when collecting data for disease control, allowing them to share information with contact tracers without individual consent.
Public interest issues affecting cooperation with contact tracing efforts
The above mentioned study ‘Digitalization of contact tracing: balancing data privacy with public health benefit’ provides the following insight, “While contact tracing and case investigation have been carefully designed to protect privacy, the huge volume of tracing which is being carried out as part of the pandemic response in the United States is highlighting potential concerns around privacy, legality, and equity.”
Concerns about data misuse, particularly with digital tools, have led to low adoption rates, even when systems are designed to be privacy-preserving. Marginalized communities, already skeptical of government surveillance, may withhold information due to fears of deportation, discrimination, or stigmatization.
Misinformation about contact tracing’s purpose (e.g., belief that it enforces quarantine punitively) undermines participation. Resource disparities also play a role: individuals lacking paid sick leave or stable housing are less likely to comply with isolation requests, perpetuating transmission in vulnerable populations.
The legislation governing data privacy in contact tracing
HIPAA permits covered entities to disclose PHI to public health authorities without individual consent for disease control purposes, as seen in COVID-19 contact tracing efforts. However, when state or local health departments conduct contact tracing outside HIPAA-covered functions, such as case management, these activities fall outside HIPAA’s scope, creating gaps in oversight.
The Privacy Act of 1974 further restricts federal agencies like the CDC from sharing personally identifiable information (PII) unless explicitly authorized. During the pandemic, agencies such as U.S. Customs and Border Protection (CBP) collaborated with the CDC under memoranda of understanding to share traveler data (e.g., names, contact details, travel history) for contact tracing, leveraging emergency exemptions to bypass typical Privacy Act limitations.
Digital contact tracing tools, such as Exposure Notification apps, exist in a legislative gray area. While the Federal Trade Commission (FTC) enforces guidelines against deceptive data practices, no federal law comprehensively governs data collected by these technologies. The CARES Act and COVID-19 executive orders temporarily eased data-sharing barriers between healthcare providers and public health agencies, but these measures lack permanence.
How healthcare organizations are impacted
Large health systems, such as the Mayo Clinic, have developed structured frameworks to manage COVID-19 contact tracing, integrating occupational health services (OHS), electronic medical records (EMRs), and human resource databases to identify exposures among staff and patients. Manual tracing processes, which initially required up to 45 minutes per case to interview infected individuals and map interactions, proved resource-intensive, particularly during surges.
To scale operations, organizations adopted digital tools like centralized exposure logs and real-time location systems, though these required upfront investments in software development and staff training. For example, algorithms were implemented to prioritize high-risk contacts, reducing delays in notification and enabling rapid isolation.
Collaboration with the CDC involves adhering to guidelines for risk stratification (e.g., classifying exposures as high, medium, or low risk) and aligning with public health mandates, such as quarantine protocols.
A Mayo Clinic Procedural study on sustainable contact tracing and exposure investigation notes, “It is extremely resource-intensive to implement contact tracing in these settings, yet it is a critical issue because these hospitals have become the epicenter of the fight against the COVID-19 pandemic…Even the Centers for Disease Control and Prevention has acknowledged that some facilities may lack the resources necessary to maintain contact tracing of HCPs.” Quarantining exposed staff strains already short-staffed units, forcing hospitals to redeploy personnel or delay non-urgent care.
FAQs
What are the types of personal information collected during contact tracing?
Contact tracing collects identifiable and sensitive data to map transmission chains and provide support. In healthcare settings, occupational health teams may also collect job roles, worksite locations, and EHR-derived data to trace workplace exposures. Digital tools, such as Exposure Notification apps, anonymize data by using Bluetooth tokens rather than GPS, though this limits contextual detail.
Does HIPAA permit healthcare providers to disclose PHI to public health authorities for contact tracing?
Yes, HIPAA permits covered healthcare providers to disclose PHI to public health authorities for purposes such as contact tracing, without obtaining written authorization from the patient. This includes sharing a patient’s name and other relevant information as required or permitted by law.
Is contact tracing confidential under HIPAA?
Yes, contact tracing is confidential. The identity of the person who tests positive and information about others who may have been exposed are kept confidential per HIPAA. Contact tracers do not reveal the identity of the infected person to their contacts.
Subscribe to Paubox Weekly
Every Friday we bring you the most important news from Paubox. Our aim is to make you smarter, faster.