Protecting personal information is a legal and ethical responsibility. Two key terms in data privacy are Personally Identifiable Information (PII) and Protected Health Information (PHI). While they share similarities, they also have distinct definitions and implications.
What is personally identifiable information (PII)?
Personally identifiable information (PII) is a broad category encompassing any data that can be used to identify an individual. It includes direct identifiers (names, Social Security numbers, and driver's license numbers) and indirect identifiers, like birthdates, ZIP codes, or even seemingly innocuous details like a person's occupation or hobbies. In essence, any information that can be used to distinguish one person from another falls under the PII umbrella.
Related: Personally identifiable information: HIPAA compliance key facts
What is protected health information (PHI)?
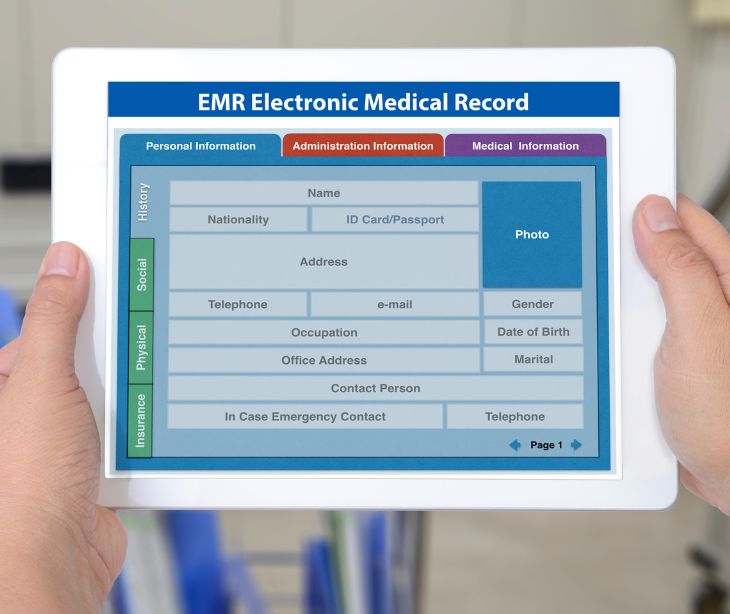
Protected health information (PHI) is a specialized subset of PII. As the name suggests, it relates to an individual's health history and medical records. PHI includes a wide range of information, such as:
- Patient names
- Medical histories
- Diagnoses
- Treatment records
- Health insurance details
- Billing records
- Laboratory test results
Related: What are the 18 PHI identifiers?
The regulatory framework for protecting PHI
In the United States, HIPAA is the primary legal framework governing the protection of PHI. HIPAA establishes the standards for the privacy and security of healthcare information. It applies to covered entities and their business associates. Failure to comply with HIPAA regulations can result in severe penalties, including substantial fines and criminal charges.
The differences between PII and PHI
Scope of information
- PII covers a wide range of personal information used in various contexts, including but not limited to financial transactions, employment, and personal communication.
- PHI is narrowly focused on an individual's health-related data, primarily encompassing information related to healthcare services, diagnoses, and medical history.
Regulatory framework
- PII protection is governed by a diverse set of laws and regulations that vary by country and region.
- PHI is subject to specific and rigorous regulation in the United States through HIPAA, which sets stringent standards for its protection.
Industry application
- PII is relevant to a broad spectrum of industries, including finance, e-commerce, marketing, and telecommunications.
- PHI is primarily associated with the healthcare and medical sectors, as it pertains exclusively to an individual's health and medical records.
Storage and retention
- PII may be stored and retained for various purposes, such as customer relationship management, marketing, and service provision. However, retention periods and storage methods can vary widely.
- PHI has strict guidelines regarding storage and retention. HIPAA mandates specific retention periods and secure storage practices to protect the confidentiality and integrity of healthcare data.
Authorized disclosures
- PII may be shared between organizations and individuals for legitimate purposes, such as customer service, business transactions, or marketing, but it must be done with consent and in compliance with relevant laws.
- PHI can only be disclosed without consent in limited circumstances specified by HIPAA, such as for treatment, payment, healthcare operations, or when required by law. Otherwise, patient consent is typically required for disclosure.
De-identification
- PII can sometimes be anonymized or de-identified to remove personally identifying characteristics, making it less sensitive.
- PHI de-identification is a complex process under HIPAA, and the resulting data must meet specific criteria to be considered de-identified and exempt from certain HIPAA requirements.
Penalties for breaches
- Breaches of PII may result in legal consequences, including fines and legal actions, depending on the severity and circumstances of the breach.
- PHI breaches are subject to strict penalties under HIPAA, including significant fines and potential criminal charges for willful negligence.
Related: Understanding HIPAA violations and breaches
How to protect PII and PHI
PII and PHI require robust protection to ensure individuals' privacy and comply with the law:
- Encryption: Use encryption technologies, like HIPAA compliant email, to secure data in transit and at rest. Encryption renders data unreadable to unauthorized users, even if they gain access.
- Access controls: Implement strict access controls, ensuring only authorized individuals can access PII or PHI. This includes user authentication, role-based access, and audit trails to monitor data access.
- Data minimization: Collect and retain only the PII or PHI necessary for legitimate business or healthcare purposes. Limit data access to what is essential.
- Regular audits and risk assessments: Conduct regular audits of data security practices and perform risk assessments to identify and address vulnerabilities promptly.
- Secure disposal: Dispose of PII and PHI securely. Shred physical documents and use secure methods to erase or destroy electronic data.
Subscribe to Paubox Weekly
Every Friday we bring you the most important news from Paubox. Our aim is to make you smarter, faster.